By Paul Sayer, Founder of Prost8.
When I was diagnosed with early-stage, treatable prostate cancer in 2018, my doctors presented me with two stark options: major surgery or a five-week course of radiotherapy, delivered five days a week. Both carried significant risks of life-changing side effects, from incontinence to erectile dysfunction, yet for years these invasive treatments have been considered the “gold standard.”
Despite being urged by my consultant to choose a traditional treatment that would have robbed me of my manhood and dignity, I embarked on extensive research to find an alternative. That research led me to better, newer, and far less invasive options in the form of highly targeted therapies available at only a few London hospitals. I was referred to world-leading urological surgeon Professor Hashim Ahmed at Imperial College Hospital, who specialises in minimally invasive prostate cancer treatments like HIFU and cryotherapy. He confirmed I was a perfect candidate. Five weeks later, I had a day-stay procedure, a catheter for a week, and was back at work — with no change to my old self.
The experience of facing such gruelling treatment options, and the anxiety over potential side effects, made me realise how many men in their fifties and beyond are forced into the same impossible choices. I wanted to make a difference for others, to show that life-saving treatment doesn’t have to come at the cost of your quality of life.
That drive led me to found Prost8, a charity dedicated to campaigning for less invasive, more advanced treatments for men with localised prostate cancer. We believe men should not have to sacrifice their lifestyle to save their lives, and thanks to remarkable advances in medical technology, that belief is now achievable.

Why We Need Change
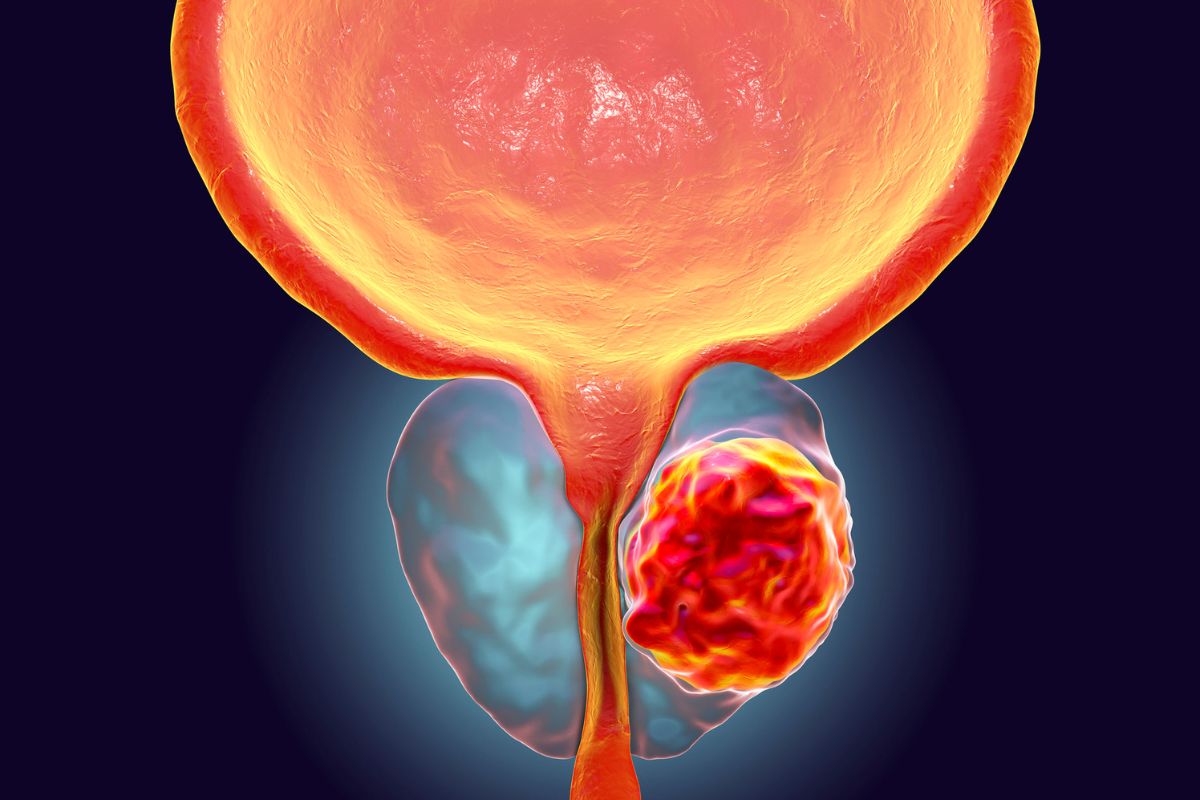
Prostate cancer affects 52,000 men in the UK every year – that’s 143 every single day, and at least 1 in 8 men will face it in their lifetime. Although survival rates are improving, the treatments offered to many men remain blunt, invasive, and unnecessarily damaging.
In 2021, NICE updated its guidance to recommend focal therapies, including high-intensity focused ultrasound (HIFU) and cryotherapy, as treatment options for localised disease. These approaches target only the diseased areas of the prostate, sparing the rest of the gland and reducing side effects.
Yet the reality remains shocking: of the 12,000 to 15,000 men who could benefit from focal treatment each year, fewer than 500 actually receive it. This is nothing short of a national disgrace. Far too many men are still directed towards outdated whole-gland treatments, even when their cancer is small and localised, meaning thousands are left with avoidable long-term complications, including erectile dysfunction and incontinence. Radical treatments for early-stage cancers can take a heavy physical and emotional toll. Recovery is gruelling, and men are left struggling not only with their health but also with their confidence, identity, and intimate relationships. As survival improves, quality of life must matter just as much as longevity!

How HIFU Technology Works
For decades, ultrasound has played a pivotal role in medicine, most commonly through safe, low-energy imaging. But it also has a therapeutic role. High-Intensity Focused Ultrasound (HIFU) concentrates powerful sound waves onto a precise spot in the prostate. These beams are thousands of times more powerful than those used in diagnostic imaging. Eliminating diseased cells while sparing healthy tissue, the treatment allows urologists to precisely contour and ablate cancerous lesions while avoiding critical structures such as nerves and the urinary sphincter, achieving targeted cancer control with significantly reduced side effects.
Unlike other procedures, HIFU is minimally invasive, usually performed under general anaesthesia, with no incisions or needles. A specialised probe inserted into the rectum both images the prostate and delivers treatment. Most patients are discharged the same day, can resume light activities within 24-48 hours, and have a temporary urinary catheter removed after 7-10 days.

Cryotherapy Explained
Cryotherapy provides another focal treatment option for men with localised prostate cancer. Rather than using heat, cryotherapy destroys cancerous tissue by freezing it. Thin, needle-like probes are carefully inserted into the prostate and cooled with argon gas, forming ice crystals that rupture cancer cells. The controlled freeze-thaw cycles further damage the tumour while sparing surrounding healthy tissue.
Like HIFU, cryotherapy is precisely targeted, reducing the risk of side effects such as incontinence and erectile dysfunction. Both procedures can be repeated if needed, and leave other treatment options open should the cancer progress.
Why This Matters for Men
For men with early-stage, localised prostate cancer, focal therapies offer the chance to treat the disease without compromising lifestyle, confidence, or intimacy. Yet awareness and availability within and outside of the healthcare system remain patchy, leaving many men unaware that these options exist.
At Prost8, we work with the UK’s leading urologists and specialist MedTech companies to expand access to these advanced treatments while also fundraising to establish HIFU units outside London that are free at the point of care, and where they are needed most.

Looking Ahead
The future of men’s health lies in precision, personalisation, and preserving quality of life. Focal therapies embody all three. But technology alone is not enough: investment, training, NHS adoption, and full patient awareness are essential to make these treatments widely available. Surviving prostate cancer should never mean living half a life.
As someone who has lived through prostate cancer, I know the fear and uncertainty it brings. But I also know the hope that innovation can offer.
The future of men’s health is being shaped today, and it’s time we gave men access to the best tools science has to offer.
About the expert
 Paul Sayer, 64, from Southend-on-Sea, Essex, was diagnosed with aggressive prostate cancer in his early 60s. Faced with the stark choice between major surgery or radiotherapy both carrying high risks of incontinence and erectile dysfunction, he sought an alternative. In July 2018, he underwent high-intensity focused ultrasound (HIFU) treatment with world-leading surgeon Professor Hashim Ahmed at Imperial College Healthcare NHS Trust. The scalpel-free procedure targeted tumour cells precisely, allowing him to avoid the long-term side effects often associated with traditional treatments. Following his successful experience, Paul founded Prost8 UK, a charity campaigning to improve access to less invasive, advanced treatments for men with localised prostate cancer and to ensure patients are informed of all their options. Learn more at prost8.org.uk
Paul Sayer, 64, from Southend-on-Sea, Essex, was diagnosed with aggressive prostate cancer in his early 60s. Faced with the stark choice between major surgery or radiotherapy both carrying high risks of incontinence and erectile dysfunction, he sought an alternative. In July 2018, he underwent high-intensity focused ultrasound (HIFU) treatment with world-leading surgeon Professor Hashim Ahmed at Imperial College Healthcare NHS Trust. The scalpel-free procedure targeted tumour cells precisely, allowing him to avoid the long-term side effects often associated with traditional treatments. Following his successful experience, Paul founded Prost8 UK, a charity campaigning to improve access to less invasive, advanced treatments for men with localised prostate cancer and to ensure patients are informed of all their options. Learn more at prost8.org.uk


